Abstract
Objection: To explore the relationship of mutation or alternative splicing events in CD19 coding region of patients underwent CD19-negative relapse after CAR-T cell therapy, as well as the predictive factors associated with relapse based on WES and RNA-seq, in the hope of explaining the mechanism of CD19-negativerelapse and improving the effect of CAR-T cell therapy.
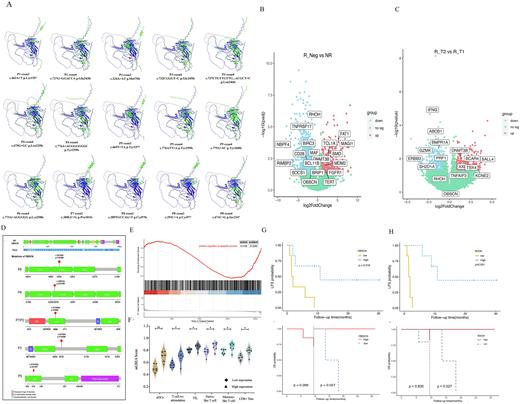
Methods: In this part of study, we collected bone marrow samples from R/R B-ALL patients underwent CD19 CAR-T cell therapy at baseline (T1) and relapse time (T2), then subjecting samples for WES and RNA-seq. Mutect and ANNOVAR software were used to detect single nucleotide variations (SNV) and indel mutations. Alphafold2 was used to predict the protein structure of CD19 after mutation. DESeq2 was used to compare the gene expression level between different groups; ssGSEA method was used to evaluate immunocyte infiltration level in each sample. Therefore, we displayed the potential mechanism of CD19-negative relapse from the aspects of leukemia cells and tumor microenvironment.
Results:CD19 exon2-4 mutations were detected in CD19-negative relapse patients at relapse time, which lead to the change of protein structure of CD19 extracellular segment (Figure 1A). The combined analysis of WES and RNA-seq revealed common mutations of OBSCN at baseline and relapse (Figure 1D), which was associated with its continued lower expression in negative-relapse group (Figure 1B-C). Meanwhile, OBSCN was enriched in positive regulation of apoptosis pathway through GO enrichment (Figure 1E). OBSCN low-expression group had poorer 1-year leukemia free survival (LFS) rate (0% vs 44.4%, P=0.016) and long-term OS rate (P=0.027) than high-expression group (Figure 1G). Moreover, RHOH, a related gene of OBSCN, which expressed lower in CD19-negative relapse patients (Figure 1B-C). The 1-year LFS rate of RHOH high-expression group was significantly better than the compared group (44.4% vs 0%, P=0.001) (Figure 1H), and the infiltration level of TN, CD8+ effector memory T cells (TEM), memory T cells (TM) and tumor infiltrating lymphocytes (TILs) were increased in RHOH high-expression group (Figure 1F).
Conclusion: Mutations of CD19 exon2-4 leads to the variation on protein structure, which hindered targeted killing process of CAR-T cells and finally resulted in CD19-negative relapse. On the other hand, OBSCN and RHOHmay play a role in promoting leukemia proliferation and decreasing apoptosis, and the lower expression of OBSCN and RHOH may be risk factors associated with CD19-negative relapse. In addition, lower expression of RHOH was unfavourable for the infiltration of TN, TEM, TM and TILs in tumor microenvironment, which lead to the weakening anti-tumor effect of immunocytes.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.